Your Lung Condition Puts You At Risk
People with a history of lung conditions, like bronchiectasis, COPD, or asthma, are more likely to develop an NTM infection. You can also get infected if you have had severe or chronic pneumonia.
That’s because the damage from these conditions can make it easier for NTM to infect your lungs, and more difficult to get rid of NTM. This puts people with lung conditions at a higher risk for getting NTM lung disease.
People with lung conditions have a higher
chance of getting NTM.
Those lung conditions include:
Bronchiectasis happens when the walls of the airways, or bronchi, thicken from chronic inflammation and/or infection, leading to the build-up of mucus. Bacteria, like NTM, often infect the lungs of people with bronchiectasis.
Approximately 50% of people with bronchiectasis may have active NTM lung disease.
COPD, or chronic obstructive pulmonary disease, is a progressive disease that makes it hard to breathe. Progressive means the disease gets worse over time. COPD can cause coughing that produces large amounts of mucus, shortness of breath, and other symptoms.
People with COPD are almost 16 times more likely to get NTM lung disease.
Asthma is a lung disease that inflames and narrows the airways. Asthma causes periods of wheezing, chest tightness, shortness of breath, and coughing. The coughing often occurs at night or early in the morning, but may occur in response to exercise or exposure to environmental triggers.
Pneumonia is a lung infection that can cause serious illness. Pneumonia can cause a cough, fever, and difficulty breathing. For most people, pneumonia may be treated at home. It often clears up with antibiotics, but older adults and people with other conditions may become very sick.
Bronchitis is inflammation of the airways, or bronchi, in the lungs. Symptoms include coughing up mucus and shortness of breath. Bronchitis can be acute or chronic.
NTM lung disease causes damage to your lungs that will only get worse with time.
Explore the damaging effects
HOW TO IDENTIFY NTM lung disease
The symptoms of NTM lung disease are similar to other lung conditions. So similar, in fact, that NTM lung disease is sometimes misdiagnosed or not diagnosed at all.
People can have NTM for months, sometimes years, without knowing it, which is why it’s important to get tested for this disease if you think you may have it. Many people have symptoms but may think it’s due to a lung condition they already have.
Ask about NTM lung disease—Think you or a loved one may have NTM lung disease? Download this discussion guide to help start a conversation about NTM with your doctor.
Download Doctor
Discussion Guide
NTM
in the United States
While NTM lung disease is considered rare, cases in the US are rising by 8% each year.
While NTM occurs throughout the US,
these 10 states report the most cases.

- Arizona
- California
- Florida
- Georgia
- Hawaii
- Illinois
- New York
- North Carolina
- Pennsylvania
- Texas
As of 2010.
Some areas of the US have higher rates of NTM lung disease. In fact, 7 out of 10 of all NTM infections in the US occur along coastal areas.
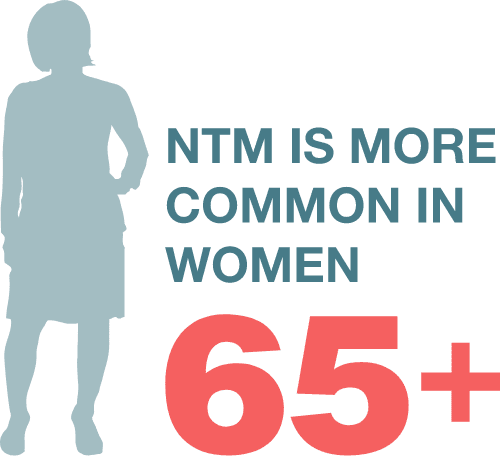
Many factors can increase your risk of NTM lung disease.
Developing NTM can be influenced by:
Where you live and the
climate in your area
Your personal health history
Your environmental exposure